
Published: 23 October 2024
Rahul H. Dave, Heidi Crayton, Augusto Miravalle, Ming-Hui Tai,
Kerri Wyse, Katherine Houghton, Abby Hitchens & Regina Berkovich
DOWNLOAD THE PDF
ABSTRACT
Introduction
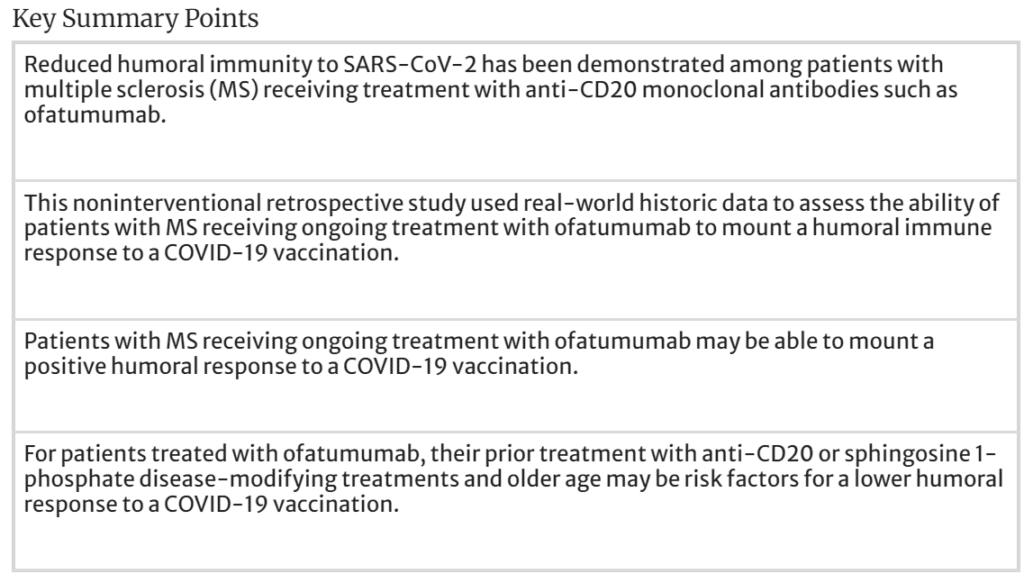
Real-world data are required to provide a greater understanding of the impact of ofatumumab on the ability to mount an effective immune response following the receipt of approved COVID-19 vaccinations. This retrospective real-world analysis aimed to describe the humoral immune response to COVID-19 vaccination during ofatumumab treatment in patients with multiple sclerosis (MS).
Methods
Data from patients with MS treated with ofatumumab who were fully vaccinated against COVID-19 infection were abstracted from medical charts at four clinical sites in the USA. Patient characteristics and humoral response were summarized descriptively. Differences in humoral response were documented on the basis of vaccination status during ofatumumab treatment (i.e., after full vaccination and after booster vaccination) and prior disease-modifying treatment (DMT) exposure (i.e., DMT naïve, prior anti-CD20/sphingosine 1-phosphate [S1P] therapy, prior non-anti-CD20/S1P therapy). The sample size precluded formal statistical analysis.
Results
Thirty-eight patients were included. The mean (standard deviation) duration of ofatumumab treatment upon data collection was 20.4 (4.6) months (treatment ongoing for 35 [92%] patients). Definitive humoral response after full vaccination was documented for 34 patients, of whom 20 (60%) were seropositive. Definitive humoral response after booster vaccination was documented among five patients, of whom three (60%) were seropositive. Among patients who were DMT naïve prior to ofatumumab (n = 15), 73% were seropositive; among patients exposed to prior anti-CD20/S1P therapy (n = 14), 33% were seropositive; and among patients exposed to prior non-anti-CD20/S1P therapy (n = 9), 56% were seropositive. Patients naïve to DMT had been living with an MS diagnosis for a shorter duration than those experienced with DMTs.
Conclusion
Patients with MS receiving ongoing treatment with ofatumumab can mount a positive humoral response to a COVID-19 vaccination. Prior treatment with anti-CD20 or S1P DMTs may be a risk factor for lower humoral response. ——
Continue reading this article below the Key Points
Introduction
Currently, 23 disease-modifying therapies (DMTs) are approved by the US Food and Drug Administration (FDA) for the treatment of multiple sclerosis (MS). Approved DMTs can be administered orally (e.g., fingolimod, teriflunomide), by injection (e.g., interferon beta, glatiramer acetate, ofatumumab), or by infusion (e.g., ocrelizumab, natalizumab) [1]. The effect of DMTs on B cell-mediated (humoral) and T cell-mediated (cell-mediated) immunity varies across DMTs.
Immunity to COVID-19 appears to depend on the combination of humoral and cell-mediated immune responses [2]. Reduced humoral immunity to SARS-CoV-2 vaccination has been demonstrated among patients with MS receiving treatment with anti-CD20 monoclonal antibodies and sphingosine 1-phosphate (S1P) modulators [3,4,5,6,7].
Treatment with anti-CD20s has been associated with severe COVID-19 in patients with relapsing–remitting MS (RRMS). In a retrospective cohort study conducted in France, treatment with anti-CD20 therapy was associated with development of severe COVID-19 in patients with RRMS (n = 51; adjusted odds ratio, 5.32 [95% CI 2.78–9.71]) [8]. Of note, these patients were older, had more neurologic disability, had received a greater number of anti-CD20 infusions, and were more frequently treated with rituximab than anti-CD20-treated patients who did not experience severe COVID-19 (n = 350); vaccination status was not shown to impact the association between anti-CD20 therapy and severe COVID-19. Further, ocrelizumab, compared with dimethyl fumarate, was associated with an increased risk of hospitalization and admission to an intensive care unit among patients with suspected or confirmed COVID-19 [9].
Humoral immune response to SARS-CoV-2 vaccines in patients with MS treated with DMTs, including anti-CD20 therapies, has also been assessed in recent years, with varying results dependent on both DMT type and vaccine type [5, 10,11,12,13,14]. These studies have shown an attenuated humoral immune response to SARS-CoV-2 vaccines in some patients treated with anti-CD20 therapies (e.g., ocrelizumab, fingolimod, ofatumumab) and support individualized patient guidance around prevention and control of COVID-19 infection.
Ofatumumab is the first self-injectable, fully human anti-CD20 monoclonal antibody. Although other anti-CD20 therapies can reduce serum immunoglobulin level concentrations, sustained long-term reductions have not been seen with ofatumumab in clinical trials [15]. Reduced immunoglobulin levels are a risk factor for infections [16]. Recent analyses of data from the long-term extension study evaluating the safety of ofatumumab (ALITHIOS [NCT03650114]) identified 603 of 1703 patients who had laboratory-confirmed COVID-19 infection. Among these cases, 92% were characterized as nonserious, and 99% were either recovered, recovered with sequalae, or were recovering from COVID-19; five (0.8%) COVID-19-infected patients had a fatal outcome [17].
This noninterventional retrospective study used historic data already contained within patient medical records at four community practices in the USA. The aim was to generate real-world data describing the immune response to COVID-19 vaccination during ofatumumab treatment.
Methods
This was a noninterventional, retrospective, observational cohort study involving the abstraction and review of pertinent data from medical records by participating physicians who completed a customized electronic case report form hosted on a secure electronic data capture system. Data were collected between August 5, 2022 and November 30, 2022. WCG Institutional review Board (IRB) approved a request for a waiver of authorization for use and disclosure of protected health information under 45 CFR 46 116(f) [2018 Requirements] 45 CFR 46.116(d) [Pre-2018 Requirements].
Eligible medical records were from patients diagnosed with MS who were aged 18 years or older upon receipt of their first COVID-19 vaccination, were fully vaccinated with any FDA-authorized COVID-19 vaccination (i.e., received two doses of a two-dose series [Pfizer, Moderna] or received one dose of a single-dose variant [Johnson & Johnson]), were receiving ofatumumab at the time of the full COVID-19 vaccination and/or first booster vaccination, and had a documented measure of humoral response at least 2 weeks after the full vaccination and/or first booster vaccination. Patients who received monoclonal antibodies to treat or prevent COVID-19 at any time between the first COVID-19 vaccination to within 6 months of the last COVID-19 vaccination (booster inclusive) were ineligible.
Data were collected on demographic characteristics, clinical characteristics, ofatumumab treatment, COVID-19 vaccination, and humoral response. Data were summarized descriptively among the total sample. Humoral response data were descriptively analyzed separately on the following basis: vaccination status while receiving ofatumumab (i.e., after full vaccination and after first booster vaccination) and prior DMT experience (i.e., DMT naïve, prior anti-CD20/S1P therapy, and prior non-anti-CD20/S1P therapy). As a result of the small sample size and exploratory nature of the study, no tests for statistical significance were conducted.
Results
Click here, to read the Results, Discussions, Figures, Charts, Conclusion and Acknowledgements
——————-
Stay informed with MS news and information - Sign-up here
For MS patients, caregivers or clinicians, Care to chat about MS? Join Our online COMMUNITY CHAT



