April 17, 2024
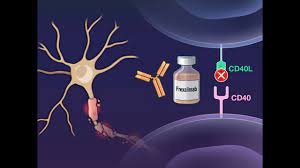
New 48-week frexalimab phase 2 data support potential for high sustained efficacy in multiple sclerosis
- Data support frexalimab as a potential first-in-class, high-efficacy, non-lymphocyte depleting treatment for relapsing multiple sclerosis
- 96% of participants receiving high-dose intravenous frexalimab had no new Gd+ T1 lesions and an annualized relapse rate of 0.04 after 48 weeks
- Sanofi has initiated global phase 3 studies of frexalimab in relapsing MS and non-relapsing secondary progressive MS
Paris, April 17, 2024. Sanofi’s CD40L antibody, frexalimab, demonstrated sustained reduction of disease activity and favorable tolerability after nearly one year in participants with relapsing multiple sclerosis. These data will be presented today at the American Academy of Neurology (AAN) 2024 Annual Meeting in Denver, Colorado, US. Results from the 12-week double-blind study period were previously published in The New England Journal of Medicine.
Patrick Vermersch, MD, PhD
University of Lille, CHU Lille, France
“These 48-week data showed that treatment with frexalimab resulted in further decreases in the number of lesions and a sustained reduction in disease activity. The preliminary clinical results are promising with a very low annual relapse rate. This strengthens the rationale for targeting CD40L in MS and supports further development of frexalimab as a potential high-efficacy therapy in relapsing MS.”
From the initial 12-week double-blind period, 97% (125/129) of study participants entered the open-label extension (OLE) of the phase 2 study. Of all participants receiving frexalimab, both on high- and low-dose regimens and participants who switched from placebo at the start of the open-label extension period (week 12), 87% (112/129) remained in the study at the 48-week cut-off. During the OLE, participants in the high- (n=50) and low-dose (n=49) arms continued to receive frexalimab 1200 mg intravenously every four weeks, or frexalimab 300 mg subcutaneously every two weeks, respectively, while those initially receiving placebo switched to the aforementioned high or low dose frexalimab treatment arms (n=12 and n=14, respectively).
Erik Wallström, MD, PhD
Global Head of Neurology Development, Sanofi
“Frexalimab represents a novel potential first-in-class treatment mechanism in multiple sclerosis designed to tackle the aspects of this disease where unmet medical needs still exist. We are applying our deep expertise to address the full spectrum of neuroinflammation and neurodegeneration to improve the lives of people living with multiple sclerosis.”
Results of the phase 2 OLE at week 48 showed:
- 96% of patients who continued receiving high-dose frexalimab and 87% of those who continued receiving low-dose frexalimab were free of Gd+ T1 lesions at week 48, respectively. Additionally, among patients who switched from placebo to high and low-dose frexalimab at the start of the OLE at week 12, declines were seen at Week 24, and 90% and 92% were free of Gd+ T1 lesions at week 48, respectively.
- The number of Gd+ T1-lesions (mean [SD]) remained low in participants who continued receiving frexalimab (high dose: 0.0 [0.2]; low dose: 0.2 [0.5]) and continued to decline in those who switched from placebo to frexalimab at week 12 (high dose: 0.2 [0.6]; low dose: 0.1 [0.3]).
- Number of and volume change of new or enlarging Gd+ T2-lesions remained low for all frexalimab treatment groups through week 48, and lymphocyte counts remained stable.
- Participants who continued receiving high-dose frexalimab experienced a low annualized relapse rate (ARR) of 0.04 (95% CI: 0.01, 0.18) over the 48-week treatment period with 96% being free of relapses. ARR in the initial low-dose arm was 0.22, and ARR in patients who switched to high and low-dose frexalimab were 0.09 and 0.40, respectively, through week 48.
Frexalimab was generally well-tolerated through week 48. The most common adverse events (≥10%) amongst all subgroups of patients receiving frexalimab during OLE until cut-off at week 48 from baseline were nasopharyngitis (n=14 [11%]), headache (n=14 [11%]) and COVID-19 (n=13 [10%]).