April 2019
Pharmacy benefit manager have a significant behind-the-scenes impact in determining drug costs and patients’ access to medications. Some experts think pharmacy benefit managers need to move their business model away from securing rebates from drugmakers and toward encouraging better value in pharmaceutical spending.
Pharmacy benefit manager have a significant behind-the-scenes impact in determining drug costs and patients’ access to medications. Some experts think pharmacy benefit managers need to move their business model away from securing rebates from drugmakers and toward encouraging better value in pharmaceutical spending.
What are pharmacy benefit managers?
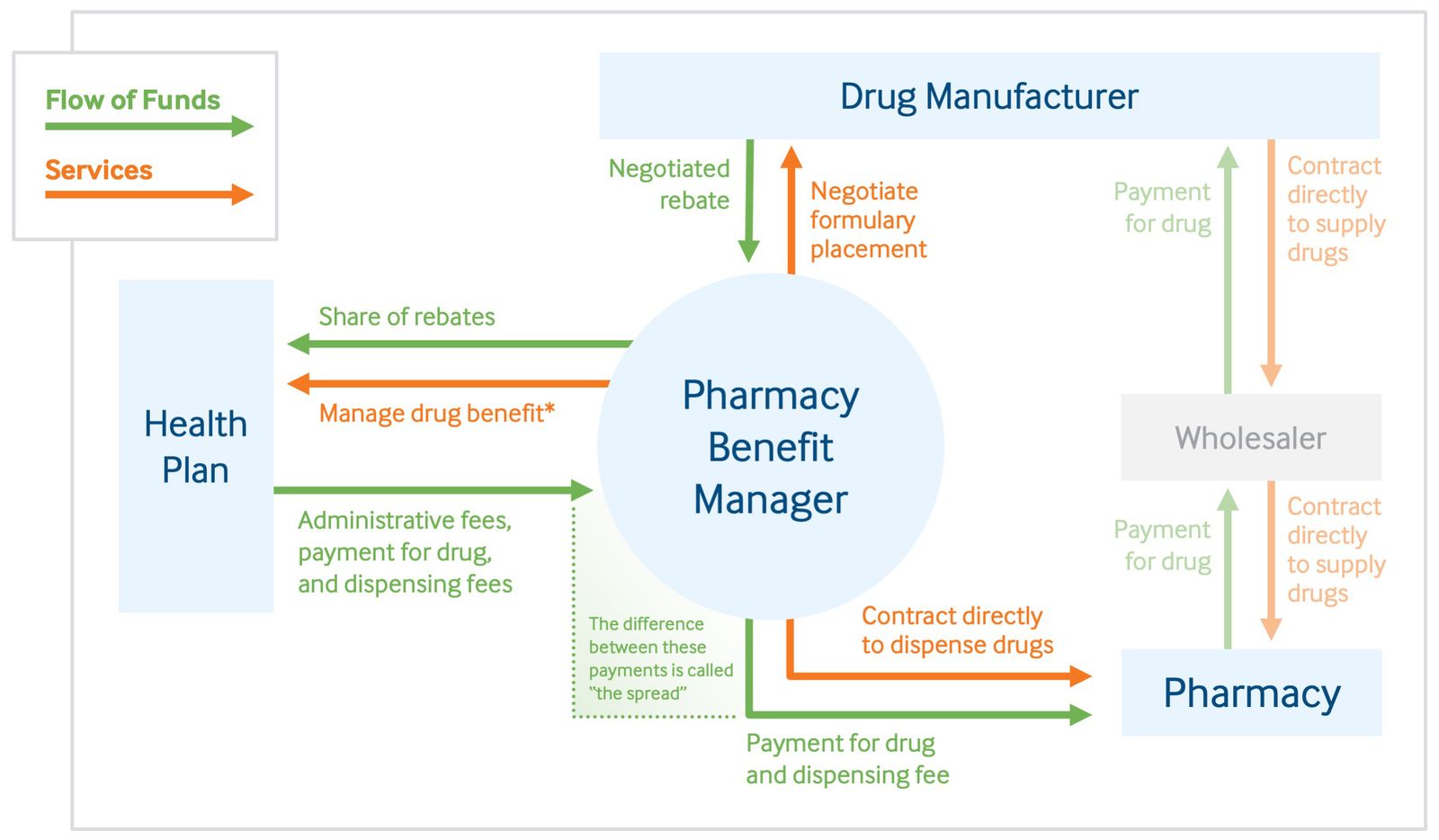
Pharmacy benefit managers, or PBMs, are companies that manage prescription drug benefits on behalf of health insurers, Medicare Part D drug plans, large employers, and other payers. By negotiating with drug manufacturers and pharmacies to control drug spending, PBMs have a significant behind-the-scenes impact in determining total drug costs for insurers, shaping patients’ access to medications, and determining how much pharmacies are paid.1 PBMs have faced growing scrutiny about their role in rising prescription drug costs and spending.
What role do PBMs play in how much we spend on prescription drugs?
PBMs operate in the middle of the distribution chain for prescription drugs. That’s because they:
- develop and maintain lists, or formularies, of covered medications on behalf of health insurers, which influence which drugs individuals use and determine out-of-pocket costs
- use their purchasing power to negotiate rebates and discounts from drug manufacturers
- contract directly with individual pharmacies to reimburse for drugs dispensed to beneficiaries.2
The federal Centers for Medicare and Medicaid Services found that PBMs’ ability to negotiate larger rebates from manufacturers has helped lower drug prices and slow the growth of drug spending over the last three years. But PBMs may also have an incentive to favor high-priced drugs over drugs that are more cost-effective. Because they often receive rebates that are calculated as a percentage of the manufacturer’s list price, PBMs receive a larger rebate for expensive drugs than they do for ones that may provide better value at lower cost. As a result, people who have a high-deductible plan or have copays based on a drug’s list price may incur higher out-of-pocket costs.3
What’s the controversy over the rebates PBMs receive from drug companies? Click here to read
Role of a Pharmacy Benefit Manager in Providing Services and Flow of Funds for Prescription Drugs
Click here to continue reading
^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^^
This Article is Provided by: #MSViewsandNews
::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::
Visit our MS Learning Channel on YouTube: http://www.youtube.com/msviewsandnews



