Last updated May 5, 2022, by Marisa Wexler, MS
✅ Fact-checked by Ines Martins, PhD
Multiple sclerosis (MS) is a neurological disorder caused by the body’s immune system erroneously attacking myelin, a fatty covering around nerve fibers. The resulting neurological damage can cause a number of MS symptoms, including fatigue, muscle spasms, balance issues, and vision problems.
Depression, trouble controlling the bladder or bowel, and difficulties with sexual health also are common in people with the disease.
Is MS fatal?
MS itself is not usually fatal. However, the disorder may increase the risk of life-threatening complications, such as severe infections or swallowing difficulties, that can set the stage for pneumonia.
On average, the lifespan for people with MS is about five to 10 years shorter than for the general population, but this gap is getting shorter as treatments and care continue to improve.
How MS progresses over time
Most people with MS experience two stages of disease. The first stage is relapsing-remitting MS (RRMS), which is characterized by episodes of new or worsening symptoms (relapses), interspersed with periods of partial or complete recovery from symptoms (remission).
Most RRMS patients will gradually enter a progressive phase of disease, called secondary progressive MS (SPMS), in which symptoms continually worsen over time, even when no relapses occur.
The time it takes to progress from RRMS to SPMS often varies substantially from person to person and potentially can be influenced by the use of disease-modifying therapies (DMTs). If left untreated, about half of RRMS patients would progress to SPMS within 10 years of disease onset. But when most patients received treatment, only about 10% converted to SPMS, and over a median of 32 years.
In approximately 15% of MS patients, the disease will enter a progressive phase immediately, with symptoms that continually get worse over time. This disease form is referred to as primary progressive multiple sclerosis (PPMS).
In general, symptoms worsen more quickly in progressive forms of MS (SPMS or PPMS) than in relapsing disease.
Although MS is often categorized as either “relapsing” or “progressive,” these categories are far from absolute and may overlap. People with progressive MS can experience disease relapses and periods of relative remission, while individuals with relapsing disease may experience some symptom progression between relapses.
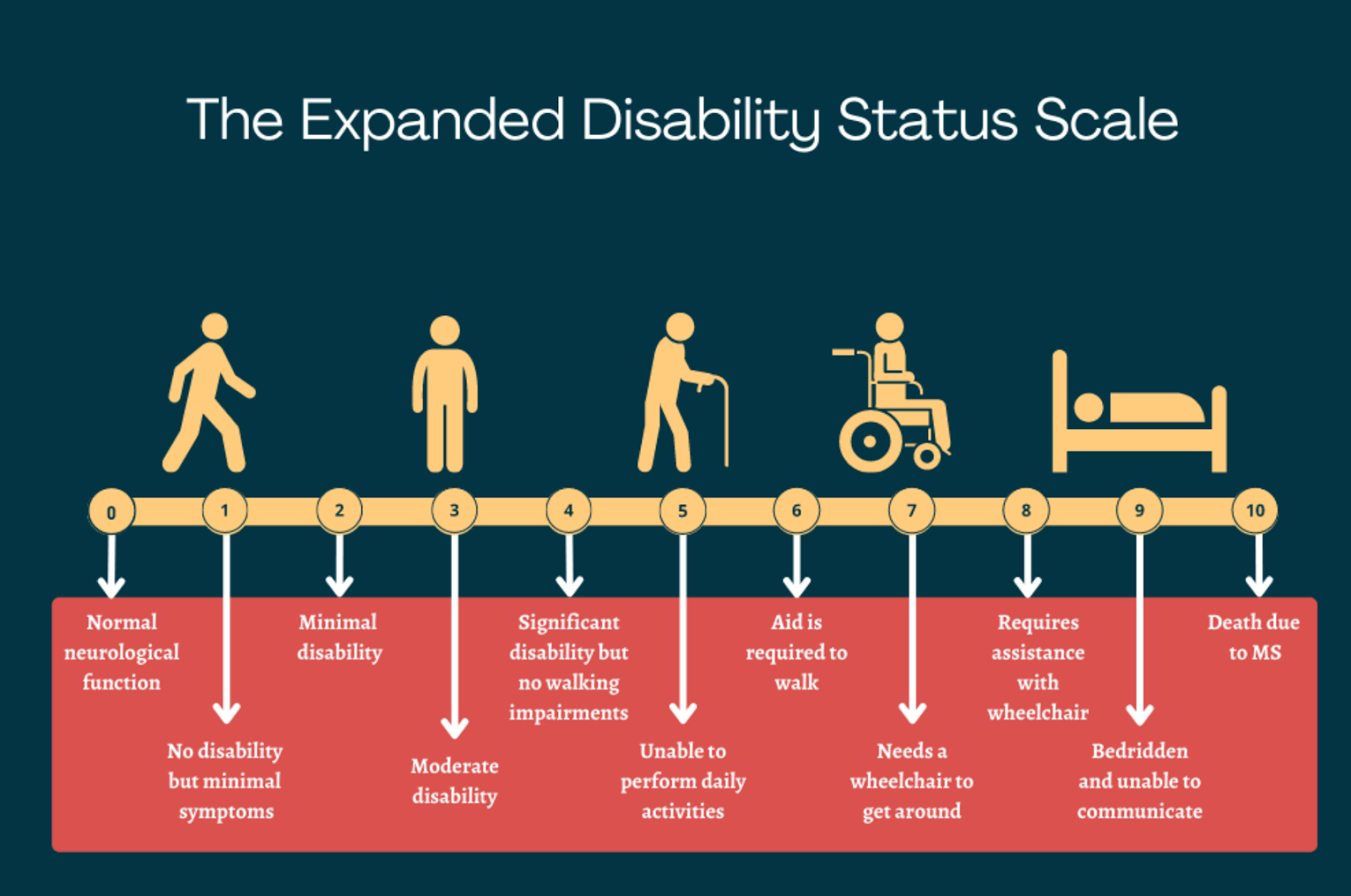
EDSS: Measuring disability progression
Disability progression in people with MS is most commonly tracked with a standardized measure called the Expanded Disability Status Scale, or EDSS. This scale ranges from 0, indicating no disability, to 10, for death. Scores increase in increments of 0.5 as disability progresses.
From scores of 0 to 4.5 in the EDSS, individuals are able to walk without any aid and their disability is measured based on impairments in functional systems. These systems represent groups of nerves responsible for specific tasks. Each is graded on a scale of 0 (no disability) to 5 or 6 (severe disability).
The EDSS assesses eight functional systems:
- pyramidal: muscle weakness or trouble moving the limbs
- visual: problems with vision
- cerebellar: tremor, loss of balance, and coordination problems
- brainstem: uncontrolled eye movements and difficulty talking or swallowing
- sensory: numbness or unusual sensations
- bowel and bladder: changes in gastrointestinal and urinary tract function
- cerebral: difficulty with thinking or memory
- other: any other neurologic finding attributed to MS
From scores of 5 to 9.5, the EDSS is assessed mainly based on an individual’s ability to walk.
Factors affecting prognosis
No two people with MS experience exactly the same symptoms or patterns of disease progression. Much like there are risk factors for developing MS, there are varying components that also can affect the disease course. These include:
- treatment
- lifestyle factors
- biological traits
- disease-intrinsic factors
- demographics, such as race and sex
Treatment
Perhaps the most important factor that affects the trajectory of MS in the modern day is treatment. Disease-modifying therapies, known as DMTs, are currently approved in the U.S. and several other countries for all the main MS types.
Beginning treatment as early as possible is highly recommended for MS patients. Long-term outcomes are generally better for patients who start treatment early in the course of their disease.
All currently approved DMTs work by reducing the inflammatory attack that drives MS. These medications have been proven in clinical trials to reduce disease activity — by lowering relapse risk, preventing new damage in the brain, and/or slowing the accumulation of disability.
Each of the available treatments has its own safety and efficacy profile, and patients are advised to talk to their healthcare team about whether certain medications might benefit them.
Lifestyle factors
Stay informed with MS news and information - Sign-up here
For MS patients, caregivers or clinicians, Care to chat about MS? Join Our online COMMUNITY CHAT