Sexual dysfunction is a common symptom in men with MS, with a prevalence that surpasses that seen in the general population and other chronic disease states.
Gavin Giovannoni – Jul 01, 2025
I am a 30-year-old man with relapsing MS. I was diagnosed when I was in my first year of University, aged 18. I presented with transverse myelitis and weakness of both legs and urinary retention. I have been on natalizumab for 12 years and have done very well. However, I have sexual problems with difficulty getting and maintaining an erection. This is affecting my relationship with my wife. Whenever I bring this up with my MS nurse or neurologist, I get fobbed off. My GP has given me Viagra, which helps, but it is unpredictable in its effects, and more often than not, it lets me down. I have gotten to the point where I now avoid sexual activity. Is there any advice you can give to help me and others like me? Thank you.
NOTE: General Substack newsletters and the microsite are free; only Q&A sessions are restricted to paying subscribers. I can’t run and maintain the MS-Selfie microsite, so I must pay people to help me do the work. If people want to ask medical questions unrelated to the Newsletters or Podcasts, they either need to become paying subscribers or email (ms-selfie@giovannoni.net) to request a complimentary subscription.
Prof G’s answers
Your email is very timely, as I was in the process of writing a chapter for the MS-Selfie microsite on sexual dysfunction (SD) in males with MS (mwMS). Sadly, SD in mwMS is a neglected topic. While the clinical presentation of MS is variable, MS can rarely present in men as SD. I have had a handful of men referred to me from the urologist with SD who are found to have MS-like lesions in their spinal cords. The following is what is currently known about the problem of SD in mwMS and how it can be managed.
Sexual Dysfunction in Men with MS
SD in mwMS is under-recognised, under-diagnosed, and undertreated. The main reasons for this are the taboos of discussing sexual dysfunction in the clinic, both from the mwMS and the HCP perspective. The response you have had from your MS nurse and neurologist is sadly rather typical.
Far from being a peripheral concern, sexual function and sexual health are essential components of overall well-being. In mwMS, the onset of SD often precipitates a decline in quality of life (QoL), negatively affecting mood, self-esteem, and intimate relationships. The distress frequently extends beyond the individual, impacting partners and contributing to marital conflict.
The aetiology of sexual dysfunction in mwMS is usually complex, variable and dynamic. In some mwMS, it is part of a relapse, and it recovers wth time. However, in most mwMS with SD, it is usually a combination of neurological, psychological, social, and cognitive factors. It is therefore vital to approach SD in mwMS from three different perspectives.
- Primary dysfunction arises directly from MS lesions within the CNS that disrupt the neural pathways governing sexual response.
- Secondary dysfunction is the collateral consequence of other MS symptoms, such as fatigue, pain, spasticity, or bladder and bowel issues, which create physical barriers to sexual activity.
- Tertiary dysfunction encompasses the psychosocial, emotional, and cultural issues that stem from living with a chronic illness, including depression, altered body image, and changes in relationships.
Sexual dysfunction is a common symptom in the mwMS, with a prevalence that surpasses that seen in the general population and other chronic disease states. Most studies report that between 50% and 90% of men living with MS will experience some form of sexual difficulty during their disease course. Despite this high prevalence, a clinical paradox exists. Despite sexual dysfunction being one of the most frequently overlooked and under-addressed symptoms of MS, it seldom gets documented and treated in mwMS. This is an example of a ‘conspiracy of silence’ where both parties in the clinical encounter overlook a significant issue affecting quality of life.
Surveys reveal that the primary barriers to discussing sexual health include time constraints during appointments, the major problem that the issue is ‘outside of my role’, lack of professional training, and perceived patient discomfort. Concurrently, patients are often reluctant to initiate these conversations due to feelings of embarrassment, shame, or a deeply held belief that sexuality is somehow incompatible with having a disability. This disconnect between the reality of the patient experience and the focus of the clinical consultation means that a treatable condition that causes significant distress is often left to fester, impacting mental health and relationships. This points to an MS healthcare need for improved clinician education, the integration of standardised screening tools into routine care, and a fundamental shift in clinical culture toward a more holistic model of well-being that values sexual health as a core component of MS management.
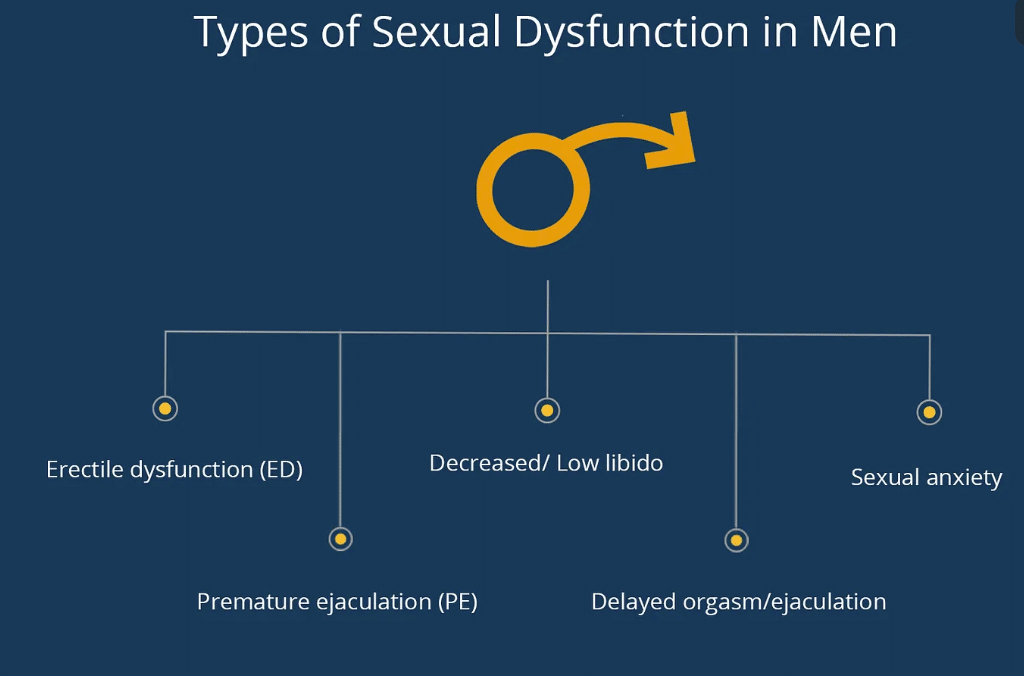
Clinical presentations of male SD
Erectile dysfunction (ED): This is the most commonly and widely studied sexual problem in men with MS. Defined as the consistent inability to achieve or maintain a penile erection sufficient for satisfactory sexual performance, ED affects a large majority of men with MS who report sexual issues, with some estimates as high as 80%. Across the entire male MS population, approximately 70% experience erectile problems at some point after an MS diagnosis.
Ejaculatory and orgasmic dysfunction: While ED receives the most attention, disorders of ejaculation and orgasm are also common and can be even more distressing for patients due to a lack of effective treatments. Studies estimate that between 35% and 50% of men with MS experience problems with ejaculation. The Male Sexual Health Questionnaire is used as a screen for dysejaculation. ED disorders manifest as:
- Delayed ejaculation or anejaculation: Difficulty or complete inability to ejaculate despite adequate stimulation.
- Premature ejaculation: Climaxing too rapidly for sexual satisfaction.
- Anorgasmia: The inability to reach orgasm.
- Altered orgasmic sensation: A less intense or less pleasurable orgasmic experience.
Disorders of libido or sexual desire: A diminished or absent interest in sex is another crucial component of SD in mwMS. Though less rigorously studied than ED, one report suggests that reduced libido affects approximately 40% of mwMS. Loss of libido is particularly complex, often arising from a combination of damage to the brain’s centres that impact desire, the secondary effect of fatigue, and tertiary psychological factors like depression and anxiety.
Altered genital sensation: The direct neurological impact of MS can manifest as abnormal sensations in the genital area. These can include numbness (decreased sensation), paraesthesias (e.g., “pins and needles”), or dysaesthesias (unpleasant or painful sensations, such as burning). These sensory disturbances can fundamentally alter the experience of sexual touch, making it less pleasurable or even painful, thereby directly interfering with arousal and orgasm.
The focus on ED in both MS research and clinical practice is driven in part by the availability of effective pharmacological treatments, which creates an incomplete picture of the patient’s experience. A management plan that successfully restores erectile function but fails to address a co-existing inability to ejaculate or a profound lack of sexual desire will ultimately fail to improve the patient’s overall sexual satisfaction and quality of life. This underscores the necessity of a thorough clinical evaluation that assesses all phases of the sexual response cycle.
The pathophysiology of sexual dysfunction in mwMS
Stay informed with MS news and information - Sign-up here
For MS patients, caregivers or clinicians, Care to chat about MS? Join Our online COMMUNITY CHAT



