
Some people with MS are on ten or more concomitant medications including gabapentin or pregabalin. Are you?
Gavin Giovannoni – Oct 08, 2024
It is pretty remarkable how many people with multiple sclerosis (pwMS) are unaware of why they are taking certain medications and the side effects and interactions of these medications. Are you one of them?
Many pwMS are prescribed concomitant medications (con-meds) to manage their many symptoms associated with a damaged or failing nervous system. There is a pharmacological treatment for virtually every MS-related symptom, whether a licensed or unlicensed medication. As a result of this, some pwMS are on ten or more con-meds. Are you?

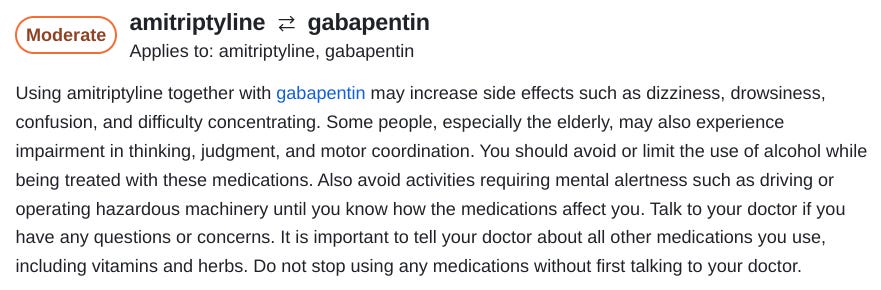
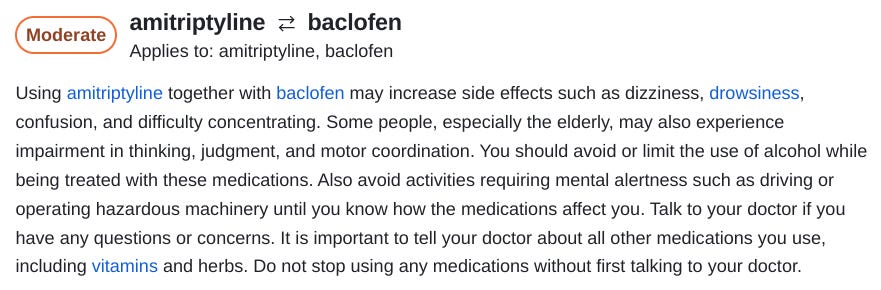
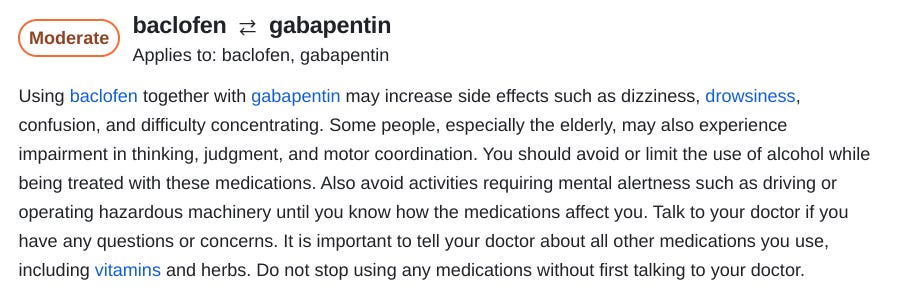
Your con-meds must be reviewed when you have your six-monthly or annual review. What many pwMS don’t realise is that many medications interact with each other, and often, side effects are not merely additive but synergistic. This is particularly common for medications that are sedating. One that I commonly encounter is the use of a sedating tricyclic antidepressant, such as amitriptyline, in combination with a gabapentinoid (gabapentin or pregabalin), and this is often given on top of an antispastic agent such as baclofen or an opioid for pain.
The following screenshots are from a commonly used online drug interaction checker. This hints at the hidden problems associated with polypharmacy.
I have already written MS-Selfie newsletters on amitryptiline and baclofen, but not on their interactions.
Please see:
A big problem in MS practice is the so-called gabapentinoids (gabapentin and pregabalin). These are used for pain management, spasticity, restless leg syndrome, nocturnal spasms, partial seizures, hiccoughs, chronic cough, pruritus & itch, paraesthesia, the MS hug, Lhermitte’s phenomenon, oscilopsia, nystagmus, sedation, anxiety, etc…
Please be aware that gabapentinoids are only licensed for seizures and pain, so most of this use is off-label. Neurologists love this drug class because the liver does not metabolise them; they are excreted unchanged in the urine and have very few adverse events that need monitoring, such as abnormal liver function tests. In reality, these drugs are another ‘dirty little secret’ of the neurologist.
I became acutely aware of how potent these medications are when I was prescribed a combination of gabapentin with morphine for my acute radicular pain when I sustained my cervical fracture in late 2020. I could not think straight or stay awake for any significant period. I also developed hallucinations on the combination, which resolved when I stopped the gabapentin. My concentration and attention were very poor whilst taking gabapentin. I remember trying to read journals during my recovery and not remembering anything I had read an hour later. My attention and recall only returned to normal when I stopped the gabapentin.
The other downside of gabapentinoids is that you develop tachyphylaxis (needing higher doses to have a treatment effect), and you usually need to increase the dose. They have a short half-life, so you must take them several times daily. For gabapentin (Neurontin), you need 3 to 4 doses per day, and for pregabalin (Lyrica), 2 to 3 doses per day.
CLICK here to continue reading from Dr. Giovannoni’s website
—————————————
Stay informed with MS news and information - Sign-up here
For MS patients, caregivers or clinicians, Care to chat about MS? Join Our online COMMUNITY CHAT



